Endometriosis: A Hidden Battle of Countless Women in India

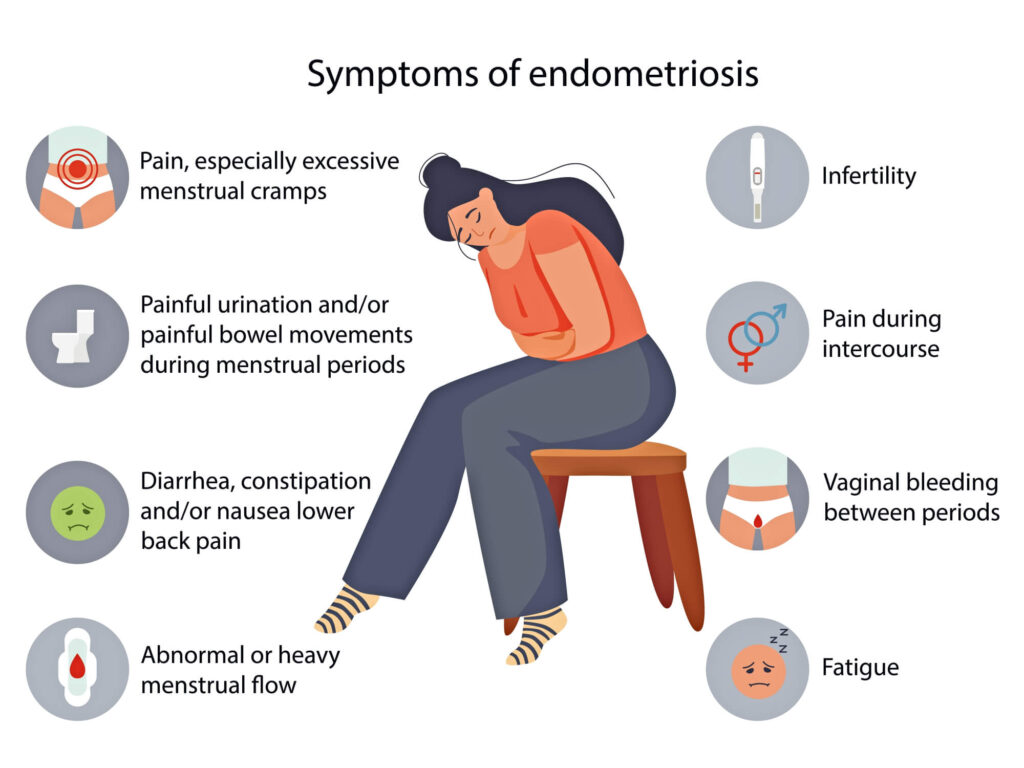
Endometriosis is a chronic gynecological condition that affects 1 in every 10 women of the reproductive age group. It occurs when the tissue of the uterine lining (womb) grows outside of the uterus. The parts most often affected are the ovaries, fallopian tubes, and pelvic sidewalls. The condition is characterized by pelvic pain ranging from mild to severe and incapacitating. The discomfort is typically felt in the pelvic area and in the lower back together with period pain. Patients can also have pain during intercourse and during opening their bowels. According to the Endometriosis Society of India, 25 million Indian women suffer from this reproductive disorder. However, it is rarely discussed and understood.
Causes of Endometriosis
The exact causes of endometriosis are not fully understood, but there are several factors that may contribute to its development.
- Retrograde menstruation: As per this theory, the menstrual blood containing endometrial cells flows backward through the fallopian tubes and into the pelvic cavity. These cells then implant and grow outside the uterus.
- Metaplasia: Metaplasia is the process by which one type of tissue transforms into another. It is believed that certain primitive cells in the pelvic region originating from the embryonal stages can undergo metaplasia and transform into endometrial-like tissue.
However, the exact cause can vary among individuals, and in many cases, the cause remains unknown. Sometimes endometriosis may run in families. Estrogen hormone stimulates the growth of endometriosis.
Consequences of Endometriosis
- The infiltrative tissue can cause pain, scarring, and adhesions of the reproductive organs as well as the organs within and outside the pelvis.
- Adhesions and scar tissues can distort and damage the ovary and fallopian tubes, leading to infertility. Pain during intercourse can also contribute to infrequent intimate relations that hamper fertility.
- This may increase the risk of developing ectopic pregnancy or infertility; such patients may be asymptomatic.
Treatment of Endometriosis
A physical examination of the patient helps in diagnosing the disease. Investigations include trans-vaginal ultrasound and MRI-Pelvis. They are conducted to identify endometriotic cysts and deep deposits that can scar the rectum. Exact treatment varies according to the condition and symptoms of the patient.
- Pain Management: Certain over-the-counter medications can help manage the pain.
- Medical therapy: Treatment with hormones such as progesterone can help relieve or eliminate endometriosis discomfort. Endometrial implants thicken, break down, and bleed as hormone levels fluctuate over the menstrual cycle. Hormone therapy may reduce endometrial tissue growth and prevent new endometrial tissue implants. Hormone therapy, however, is not curative for endometriosis.
- Surgery: Surgery is done to remove the diseased tissue completely. It involves restoring normal anatomy and organ function. Surgery is the only modality of treatment that improves fertility. Surgery for endometriosis is complex and should only be done by an expert surgeon.
If left undiagnosed and untreated, endometriosis can worsen over time, leading to serious symptoms, and more complex treatments. It can also have an impact on mental health, leading to depression, anxiety, and other psychological issues. If you have endometriosis and believe it is affecting your mental and emotional well-being, consider getting into a support group for women experiencing similar issues. Sometimes just talking to other women who understand your feelings and experiences might help.
About the author-Dr. Sujata Datta, Gynaecology, Fortis Anandapur
